What Is the Difference Between a Wound and an Ulcer?
Discover the key differences between a wound and an ulcer in wound care. Learn causes, healing challenges, and treatment strategies to improve patient outcomes.
admin
10/27/20255 min read

Patients and clinicians often use the words “wound” and “ulcer” interchangeably, but the terms describe overlapping, not identical, concepts. Understanding their difference helps with accurate assessment, faster diagnosis, and better treatment choices in wound care. This post explains the practical differences, gives clear examples, and outlines how the causes and care differ.
Short answer
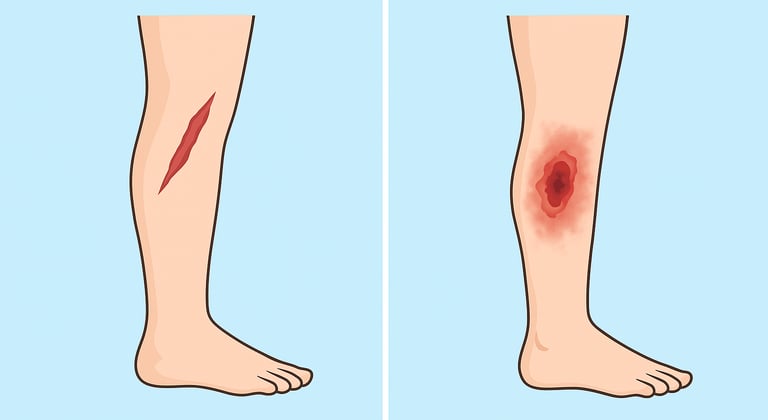
A wound is any break in the skin or deeper tissue caused by injury, surgery, or disease. Think of cuts, lacerations, surgical incisions, burns, and ulcers.
An ulcer is a type of wound that usually reflects tissue breakdown from internal or ongoing causes (for example, poor blood flow, venous hypertension, pressure, or metabolic disease). Ulcers are often chronic and may take a long time to heal.
Put another way: every ulcer is a wound, but not every wound is an ulcer.
Definitions and clinical framing
Many authorities define wounds broadly and reserve the term ulcer for lesions with certain underlying causes or chronic behavior:
A wound: “a disruption of normal anatomic structure and function” that may be acute (sudden injury or surgery) or chronic (fails to heal in an expected time).
An ulcer: commonly used to describe localized skin and tissue loss that develops because of ongoing internal or environmental stressors. For example, pressure (pressure injury), venous hypertension (venous leg ulcer), ischemia from peripheral arterial disease (arterial ulcer), or neuropathic breakdown in diabetes (diabetic foot ulcer). Many clinical guidelines treat ulcers as a subset of chronic wounds.
Regulatory and guideline documents sometimes make the distinction explicit because it affects coding, reporting, and care pathways. For example, US Medicare guidance and clinical definitions differentiate acute post-injury wounds from chronic ulcers driven by systemic disease.
Typical examples to illustrate the difference
Acute wound (not an ulcer): a cut from a kitchen accident or a surgical incision. These usually have a clear event, and with appropriate care they move through normal healing phases and close in days to weeks.
Ulcer (a chronic wound type):
Diabetic foot ulcer (DFU): arises from neuropathy, repetitive pressure, and sometimes poor blood flow; it often becomes chronic and risks infection and amputation.
Venous leg ulcer (VLU): results from chronic venous insufficiency and prolonged ambulatory venous hypertension; compression therapy targets the underlying cause.
Pressure ulcer / pressure injury: caused by prolonged pressure and shear over bony prominences; staging systems classify severity and guide pressure-relief strategies.
Arterial (ischemic) ulcer: occurs from poor arterial blood flow; revascularization may be required to help healing.
These ulcer types are often grouped under chronic wounds because they frequently fail to progress through the normal repair sequence without targeted intervention.
Why ulcers often become chronic
Ulcers tend to persist because the underlying driver of tissue breakdown has not been addressed. Common barriers include:
Poor perfusion / ischemia (arterial disease) limiting oxygen and nutrient delivery.
Sustained pressure or shear (pressure injuries) that continues to damage the same area.
Venous hypertension and edema causing capillary leak and impaired healing (venous ulcers).
Neuropathy and repetitive trauma (diabetic foot ulcers) leading to unnoticed injury and breakdown.
Persistent microbial biofilm in the wound bed, which resists host defenses and topical treatments and keeps the wound in a prolonged inflammatory state. Biofilm is a major factor in many non-healing ulcers.
Systemic issues such as poor nutrition, uncontrolled diabetes, renal disease, or immunosuppression.
Because ulcers often reflect continuing disease processes, successful care usually requires both local wound management (debridement, moisture balance, infection control) and correction of the root cause (offloading, compression, revascularization, glycemic and nutritional optimization).
Practical differences in assessment and treatment
When you approach a wound versus an ulcer, think about cause and context:
Assessment for an acute wound focuses on the injury event, bleeding control, tetanus status, wound cleaning, and closure approach (suture, adhesive, or allowing to heal by secondary intention). Routine dressing and follow-up are often enough.
Assessment for an ulcer includes the above plus investigations targeted to the suspected driver: vascular studies (ABI/toe pressure), venous duplex, neuropathy testing, nutritional screen, and consideration of tissue cultures or imaging for osteomyelitis. Early multidisciplinary input (vascular surgery, podiatry, wound clinic, infectious diseases, dietetics) is frequently helpful.
Treatment differences commonly seen in practice:
Acute wound: clean, protect, and allow healing; consider closure.
Ulcer: remove necrotic tissue (regular debridement), manage biofilm/infection, apply disease-specific therapy (compression for VLUs, offloading for DFUs, revascularization for ischemic ulcers), and address systemic factors. Advanced therapies (skin substitutes, negative-pressure wound therapy, hyperbaric oxygen) may be considered after optimizing the wound bed and treating root causes.
Simple rules clinicians can use
If the lesion followed a single, external trauma (cut, burn, surgical incision), start with acute wound care and monitor for expected progress.
If the lesion arises without a clear single injury (for example, a slowly enlarging sore on the lower leg, a recurrent foot lesion in a person with diabetes, or a pressure point breakdown), treat the lesion as an ulcer and assess for underlying causes.
Set a review timeline: if a wound is not showing measurable improvement after an appropriate, documented trial of care (commonly 2–4 weeks), consider escalation or specialist referral. This is especially important for suspected ulcers.
Final note
Language and classification evolve across specialties and regions. Some historical definitions were stricter (ulcer = internal cause, wound = external cause), but modern practice focuses on pathophysiology and care needs rather than rigid labels. Using precise assessment and documenting the suspected cause helps ensure patients receive the right investigations and timely specialist care.
See also
What Are the Different Types of Wounds? A Practical Guide
Best Practices for Chronic Wound Care: How to Assess Foot Ulcers Effectively
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
How Often Should Wound Dressings Be Changed? Best Practices for Healing
Wound Care Guide: How to Tell Colonization from True Infection
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Falanga V, Isseroff RR, Soulika AM, Romanelli M, Margolis D, Kapp S, Granick M, Harding K. Chronic wounds. Nature Reviews Disease Primers. 2022 Jul 21;8(1):50. doi: 10.1038/s41572-022-00377-3. PMID: 35864102; PMCID: PMC10352385. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10352385/
Zaidi SRH, Sharma S. Pressure Ulcer. [Updated 2024 Jan 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553107/
Diban F, Di Lodovico S, Di Fermo P, D'Ercole S, D'Arcangelo S, Di Giulio M, Cellini L. Biofilms in Chronic Wound Infections: Innovative Antimicrobial Approaches Using the In Vitro Lubbock Chronic Wound Biofilm Model. Int J Mol Sci. 2023 Jan 5;24(2):1004. doi: 10.3390/ijms24021004. PMID: 36674518; PMCID: PMC9862456. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9862456/
Wang X, Yuan CX, Xu B, Yu Z. Diabetic foot ulcers: Classification, risk factors and management. World J Diabetes. 2022 Dec 15;13(12):1049-1065. doi: 10.4239/wjd.v13.i12.1049. PMID: 36578871; PMCID: PMC9791567. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9791567/
https://www.wjgnet.com/1948-9358/full/v13/i12/1049.htm?appgw_azwaf_jsc=90x30AAxxmEPJHyc-KA7SmEIrEpnzKpD9YUigy6ifeYvan Netten JJ, Bus SA, Apelqvist J, et al. Definitions and criteria for diabetes‐related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev. 2023;e3654. https://doi.org/10.1002/dmrr.3654 https://iwgdfguidelines.org/wp-content/uploads/2023/05/DMRR3654.pdf
Cavallo I, Sivori F, Mastrofrancesco A, Abril E, Pontone M, Di Domenico EG, Pimpinelli F. Bacterial Biofilm in Chronic Wounds and Possible Therapeutic Approaches. Biology. 2024; 13(2):109. https://doi.org/10.3390/biology13020109 https://www.mdpi.com/2079-7737/13/2/109
Hermans MH. wounds and ulcers: back to the old nomenclature . Wounds. 2010 Nov;22(11):289-93. PMID: 25901519. https://pubmed.ncbi.nlm.nih.gov/25901519/
Centers for Medicare & Medicaid Services. Response to Comments: Wound and Ulcer Care. https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=58903&ver=6
Wei, Di1; Zhu, Xiao-Mei1; Chen, Yong-Yi2; Li, Xu-Ying3; Chen, Yu-Pan1; Liu, Hua-Yun1; Zhang, Min3. Chronic wound biofilms: diagnosis and therapeutic strategies. Chinese Medical Journal 132(22):p 2737-2744, November 20, 2019. | DOI: 10.1097/CM9.0000000000000523 https://journals.lww.com/cmj/fulltext/2019/11200/chronic_wound_biofilms__diagnosis_and_therapeutic.13.aspx
Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):e3276. https://doi.org/10.1002/dmrr.3276
https://iwgdfguidelines.org/wp-content/uploads/2020/11/Hinchliffe_et_al-2020-IWGDF-PAD-guideline.pdf
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
