The Role of Nutrition in Wound Care: Best Foods for Healing
Discover how nutrition impacts wound healing. Learn the best foods, vitamins, and supplements that support faster recovery and stronger tissue repair.
admin
10/21/20259 min read
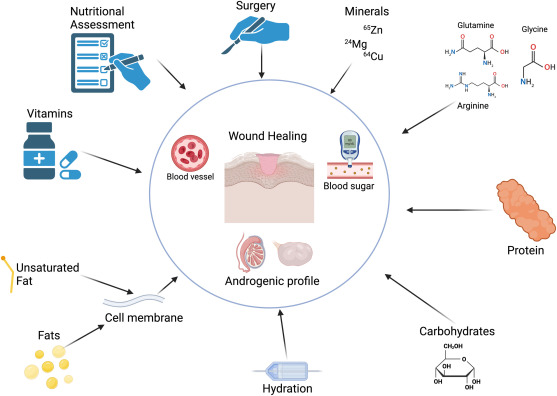
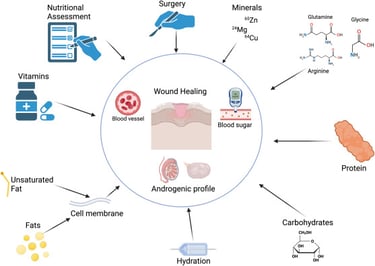
Good nutrition is a powerful, and often underused, tool in wound care. When wounds are slow to heal, clinicians commonly look at the wound bed, infection status, blood flow, and offloading. It’s equally important to check the patient’s nutritional status. Poor intake, protein deficiency, or missing micronutrients can delay collagen formation, impair immune function, and prolong inflammation. This guide explains which nutrients matter, practical food- and meal-ideas that support repair, evidence for supplements, and realistic tips clinicians and patients can use right away.
Why nutrition matters for wound healing
Wound healing is energy- and protein-intensive. Cells need amino acids to build new tissue, vitamins and minerals to make collagen and control oxidative stress, and energy to fuel the inflammatory and proliferative phases of healing. Malnutrition is associated with delayed healing, higher infection rates, and longer hospital stays. For many chronic wounds (pressure injuries, venous leg ulcers, diabetic foot ulcers), addressing nutrition is a necessary part of a complete care plan.
The most important nutrients for wound repair
Below are the nutrients most strongly linked to wound healing, with plain-language notes on food sources and the evidence behind them.
1. Protein: the single most important macronutrient
Why it matters: Amino acids are the building blocks for collagen, granulation tissue, and immune proteins. Protein also helps preserve lean body mass in catabolic states. Wounds increase protein needs; many guideline documents and reviews highlight protein repletion as a first step.
Practical targets: For patients with wounds, recommended protein intakes are often higher than for healthy adults. Clinically used ranges are roughly 1.2–1.5 g/kg/day, sometimes more for severely catabolic patients, tailored to renal function and other comorbidities. Oral nutritional supplements (ONS) that are protein-enriched can help reach targets.
Good foods: Lean meats (chicken, turkey), fish, eggs, dairy (Greek yogurt, cottage cheese), legumes (lentils, chickpeas), tofu, tempeh, and protein-fortified drinks. Nuts and seeds provide protein plus healthy fats. Health
2. Vitamin C: essential for collagen synthesis
Why it matters: Vitamin C (ascorbic acid) is required for the enzymatic steps that cross-link collagen; deficiency impairs collagen formation and wound strength. Several systematic reviews and trials report improved healing parameters with vitamin C supplementation in some wound types (particularly pressure ulcers), though study sizes and designs vary.
Practical targets & foods: Aim for adequate intake (the RDA is ~75–90 mg/day for adults, but some trials used higher supplemental doses when deficiency or poor healing was present). Rich food sources: citrus fruits, strawberries, kiwi, bell peppers, broccoli, and tomatoes. If intake is low or deficiency is suspected, consider supplementation under clinical supervision.
3. Zinc: supports cell proliferation and immune function
Why it matters: Zinc is needed for DNA synthesis, cell division, and immune competence. Trials in diabetic foot ulcers and pressure injuries suggest zinc supplementation can improve some wound parameters in deficient or at-risk patients, although evidence is mixed and baseline zinc status matters. Excess zinc can be harmful, so supplementation should be targeted.
Foods: Oysters, red meat, poultry, beans, nuts, whole grains, and dairy. Typical supplemental dosing in trials varies; check baseline labs when possible.
4. Arginine and conditionally essential amino acids
Why it matters: Arginine is a precursor for nitric oxide, which supports blood flow and immune cell function. Some oral nutritional supplements that are enriched with arginine (often combined with omega-3 fatty acids and nucleotides) have been linked to improved healing of pressure ulcers and surgical wounds in clinical studies and reviews. Evidence suggests these formulas may be helpful in selected patients, particularly those who are malnourished or have pressure injuries.
Foods & supplements: Arginine-rich foods include meat, poultry, dairy, nuts, and seeds. Specialized ONS may be the most practical way to deliver clinical doses used in trials.
5. Omega-3 fatty acids (EPA/DHA) and inflammation modulation
Why it matters: Omega-3s modulate inflammation and may support the resolution phase of healing. Some trials and reviews suggest benefits for venous leg ulcers and improved wound parameters when combined with conventional care, but other lab data indicate complex effects (timing and dose may matter). Use with clinical judgment. They are not universal wound “cures.”
Foods: Fatty fish (salmon, mackerel, sardines), walnuts, chia seeds, flaxseed (ALA), and algae-derived supplements (for vegan options).
6. Key B vitamins, vitamin A, vitamin D, and antioxidants
B vitamins (especially B12 and folate) support cell proliferation and red blood cell production; deficiency may indirectly impair healing.
Vitamin A helps epithelialization and immune function; topical and systemic forms have research support in selected situations.
Vitamin D has roles in immunity and may influence outcomes in some chronic wounds; low vitamin D is common in some populations.
Antioxidants (vitamin E, polyphenols): evidence is variable; some compounds may reduce oxidative stress but clinical benefit is mixed and depends on wound type and patient context.
Foods: Leafy greens, dairy or fortified plant milks, eggs, liver (sparingly), nuts, fruits, and a range of colorful vegetables provide many of these micronutrients.
Oral nutritional supplements (ONS) — when food alone isn’t enough
When patients can’t meet increased needs with regular meals (poor appetite, dysphagia, increased metabolic demand), ONS can fill the gap. Clinical studies and reviews have shown that protein- and arginine-enriched formulas (often with vitamin C, zinc, and omega-3s) may improve healing of pressure injuries and other chronic wounds when used as part of comprehensive care. Choose formulas with demonstrated clinical use and monitor for tolerance and glucose control in people with diabetes.
Evidence summary & what the research supports
Protein repletion and correction of malnutrition are broadly supported as essential for wound healing; many guideline groups emphasize assessing and treating malnutrition.
Vitamin C and zinc show positive signals in systematic reviews for certain wound types (pressure ulcers, some chronic wounds). Benefit seems more likely when deficiency is present and when supplements are used as part of a package of care.
Arginine-containing ONS and immunonutrition formulas have evidence of benefit for pressure ulcers and some surgical wounds, particularly in malnourished patients.
Omega-3s and other anti-inflammatory nutrients show promise in some studies (for venous ulcers and modulating inflammation), but the evidence is mixed and timing/dose matter.
Overall: nutrition is necessary but usually not sufficient alone. It is an essential adjunct to debridement, infection control, offloading, revascularization, and appropriate dressings.
Practical, clinician-ready nutrition checklist for wound patients
Screen every patient for malnutrition (weight loss, low BMI, poor intake). Early detection matters.
Estimate energy and protein needs. Typical starting points: 25–35 kcal/kg/day and 1.2–1.5 g protein/kg/day for most patients with chronic wounds; adjust for obesity, renal failure, or hypercatabolism.
Check key labs if available: albumin/prealbumin (limited as acute markers), vitamin D, vitamin C if deficiency suspected, and consider zinc/iron studies when indicated. Use labs alongside clinical assessment.
Start food-first strategies: small frequent protein-rich meals, nutrient-dense snacks (Greek yogurt with berries, nut butter on whole-grain toast, smoothies with protein powder and fruit), and include colorful vegetables for vitamin C and antioxidants.
If intake is inadequate, add an ONS focused on protein and, if clinically indicated, formulas enriched with arginine, omega-3s, vitamin C, and zinc. Reassess after 2–4 weeks.
Address modifiable barriers: dental issues, nausea, swallowing problems, food insecurity, polypharmacy affecting appetite. Collaborate with dietitians, social work, and primary care.
Practical food ideas (patient-friendly)
Morning: Greek yogurt + berries + tablespoon ground flaxseed (protein + vitamin C + omega-3 ALA).
Mid-morning snack: a smoothie (milk or fortified plant milk, protein powder, banana, spinach).
Lunch: grilled chicken or tofu salad with bell peppers, tomatoes, avocado, olive oil (protein, vitamin C, healthy fats).
Afternoon snack: cottage cheese with sliced peach or handful of mixed nuts.
Dinner: baked salmon (omega-3) with quinoa (protein) and steamed broccoli (vitamin C).
Night snack: milk or fortified yogurt for extra protein and calories.
For patients with poor appetite: small, frequent nutrient-dense portions, oral nutritional drinks between meals, and avoid long fasting periods.
Safety cautions and when to test first
Don’t blindly supplement: high-dose zinc can interfere with copper, excess vitamin A can be toxic, and some supplements interact with medications. Check labs and consult a dietitian or clinician before high-dose supplements.
Diabetes: many ONS contain carbohydrate. Track glucose and choose formulas with appropriate carb/protein balance. Monitor glycemic control.
Renal impairment: protein and electrolyte targets change. Coordinate with nephrology/dietitians.
Final takeaways
Assess nutrition early in every patient with a chronic or complex wound. Malnutrition is common and correctable.
Prioritize protein and correct micronutrient deficiencies (vitamin C, zinc, vitamin D) when present. Use food-first approaches and add targeted ONS when intake is inadequate.
Consider specialized ONS (arginine/omega-3/vitamin C/zinc) for pressure injuries and selected surgical wounds when patients are malnourished or not improving with standard care.
Nutrition is one pillar of wound care — alongside debridement, infection control, revascularization, offloading, and appropriate dressings. Address the whole patient.
See also
When to Use Skin Substitutes or Grafts for Non-Healing Wounds
Stem Cells, Exosomes, and Biologics: Do They Work in Wound Care?
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
Why Diabetic Foot Wounds Heal Slowly: Top Factors That Delay Recovery
How Often Should Wound Dressings Be Changed? Best Practices for Healing
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Allan Carlos Soares do Espírito Santo, Clara Sandra de Araújo Sugizaki, Alcides Corrêa de Morais Junior, Nara Aline Costa, Maria Marcia Bachion, João Felipe Mota, Impact of oral nutritional supplement composition on healing of different chronic wounds: A systematic review, Nutrition, Volume 124, 2024, 112449, ISSN 0899-9007, https://doi.org/10.1016/j.nut.2024.112449 https://www.sciencedirect.com/science/article/abs/pii/S0899900724000996
Weimann A, et al. ESPEN practical guideline: Clinical nutrition in surgery. Clinical Nutrition. 2021. vol 40, iss 7. pgs 4745-4761. https://www.clinicalnutritionjournal.com/article/S0261-5614(21)00178-3/fulltext
https://www.espen.org/files/ESPEN-Guidelines/ESPEN_practical_guideline_Clinical_nutrition_in_surgery.pdfMunoz N, Posthauer ME. Nutrition strategies for pressure injury management: Implementing the 2019 International Clinical Practice Guideline. Nutrition in Clinical Practice. 2022 Jun;37(3):567-582. doi: 10.1002/ncp.10762. Epub 2021 Aug 31. PMID: 34462964. https://pubmed.ncbi.nlm.nih.gov/34462964/ https://aspenjournals.onlinelibrary.wiley.com/doi/abs/10.1002/ncp.10762
Wang X, Yu Z, Zhou S, Shen S, Chen W. The Effect of a Compound Protein on Wound Healing and Nutritional Status. Evidence-Based Complementary and Alternative Medicine. 2022 Mar 24;2022:4231516. doi: 10.1155/2022/4231516. PMID: 35368770; PMCID: PMC8970868. https://pmc.ncbi.nlm.nih.gov/articles/PMC8970868/
Bechara N, Flood VM, Gunton JE. A Systematic Review on the Role of Vitamin C in Tissue Healing. Antioxidants (Basel). 2022 Aug 19;11(8):1605. doi: 10.3390/antiox11081605. PMID: 36009324; PMCID: PMC9405326. https://pmc.ncbi.nlm.nih.gov/articles/PMC9405326/
Dadfar, Reza1,2; Khorsandi, Layasadat3,4; Goujani, Reza5; Mousavi, Seyyed Farid6; Aslani, Zahra7. Therapeutic Utilization of Zinc Supplementation Concurrent with Ozone Therapy Ameliorates Diabetic Foot Ulcer and Attenuates Serum Level of C-Reactive Protein- A Case Report Study. Advanced Biomedical Research 12(1):18, January 2023. | DOI: 10.4103/abr.abr_11_22 https://journals.lww.com/adbm/fulltext/2023/01270/therapeutic_utilization_of_zinc_supplementation.18.aspx
McDaniel JC, Belury M, Ahijevych K, Blakely W. Omega-3 fatty acids effect on wound healing. Wound Repair and Regeneration. 2008 May-Jun;16(3):337-45. doi: 10.1111/j.1524-475X.2008.00388.x. PMID: 18471252; PMCID: PMC2967211. https://pmc.ncbi.nlm.nih.gov/articles/PMC2967211/
Seth I, Lim B, Cevik J, Gracias D, Chua M, Kenney PS, Rozen WM, Cuomo R. Impact of nutrition on skin wound healing and aesthetic outcomes: A comprehensive narrative review. JPRAS Open. 2024 Jan 23;39:291-302. doi: 10.1016/j.jpra.2024.01.006. PMID: 38370002; PMCID: PMC10874171. https://pmc.ncbi.nlm.nih.gov/articles/PMC10874171/.
https://www.jprasopen.com/article/S2352-5878(24)00007-X/fulltextGomes F, et al. ESPEN guideline on nutritional support for polymorbid internal medicine patients Clinical Nutrition. 2018. vol 37. iss 1. p336-353. https://www.espen.org/files/ESPEN-Guidelines/ESPEN_guidelines_on_nutritional_support_for_polymorbid_internal_medicine_patients.pdf
https://www.clinicalnutritionjournal.com/article/S0261-5614(17)30236-4/fulltextCitty SW, Cowan LJ, Wingfield Z, Stechmiller J. Optimizing Nutrition Care for Pressure Injuries in Hospitalized Patients. Adv Wound Care (New Rochelle). 2019 Jul 1;8(7):309-322. doi: 10.1089/wound.2018.0925. Epub 2019 Jul 2. PMID: 31832278; PMCID: PMC6906754. https://pmc.ncbi.nlm.nih.gov/articles/PMC6906754/ https://www.liebertpub.com/doi/10.1089/wound.2018.0925
Momen-Heravi M, Barahimi E, Razzaghi R, Bahmani F, Gilasi HR, Asemi Z. The effects of zinc supplementation on wound healing and metabolic status in patients with diabetic foot ulcer: A randomized, double-blind, placebo-controlled trial. Wound Repair and Regeneration. 2017 May;25(3):512-520. doi: 10.1111/wrr.12537. Epub 2017 May 9. PMID: 28395131. https://pubmed.ncbi.nlm.nih.gov/28395131/
Alexander JW, Supp DM. Role of Arginine and Omega-3 Fatty Acids in Wound Healing and Infection. Advances in Wound Care (New Rochelle). 2014 Nov 1;3(11):682-690. doi: 10.1089/wound.2013.0469. PMID: 25371851; PMCID: PMC4217020. https://pmc.ncbi.nlm.nih.gov/articles/PMC4217020/
Mackay E. Malnutrition and wound healing. Wound Care Canada (2019). https://healthassociation.ns.ca/wp-content/uploads/2023/03/WCC-Fall-2019-v17n3-FINAL-p.33-37-Malnutrition.pdf
Ju M, Kim Y, Seo KW. Role of nutrition in wound healing and nutritional recommendations for promotion of wound healing: a narrative review. Annals of Clinical Nutrition and Metabolism. 2023;15(3):67-71. https://www.e-acnm.org/upload/pdf/acnm-15-3-67.pdf
https://e-acnm.org/journal/view.php?doi=10.15747/ACNM.2023.15.3.67Skórka M, Bazaliński D, Więch P, Kłęk S, Kozieł D, Sierżantowicz R. Nutritional Status in a Group of Patients with Wounds Due to Diabetic Foot Disease and Chronic Venous Insufficiency. Journal of Clinical Medicine. 2024 Dec 25;14(1):43. doi: 10.3390/jcm14010043. PMID: 39797126; PMCID: PMC11722122. https://pmc.ncbi.nlm.nih.gov/articles/PMC11722122/
Bechara N, Flood VM, Gunton JE. A Systematic Review on the Role of Vitamin C in Tissue Healing. Antioxidants (Basel). 2022 Aug 19;11(8):1605. doi: 10.3390/antiox11081605. PMID: 36009324; PMCID: PMC9405326. https://pmc.ncbi.nlm.nih.gov/articles/PMC9405326/
Serini S, Calviello G. New Insights on the Effects of Dietary Omega-3 Fatty Acids on Impaired Skin Healing in Diabetes and Chronic Venous Leg Ulcers. Foods. 2021; 10(10):2306. https://doi.org/10.3390/foods10102306
https://www.mdpi.com/2304-8158/10/10/2306ASPEN clinical guidelines and standards: https://nutritioncare.org/clinical-resources/guidelines-standards/
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
Factors that potentially influence wound healing and aesthetic outcomes. [JPRAS OPEN]
