The Difference Between Acute and Chronic Wounds — A Practical Guide
Learn the key differences between acute and chronic wounds, including causes, healing stages, and treatment strategies to improve wound care outcomes.
admin
10/26/20255 min read
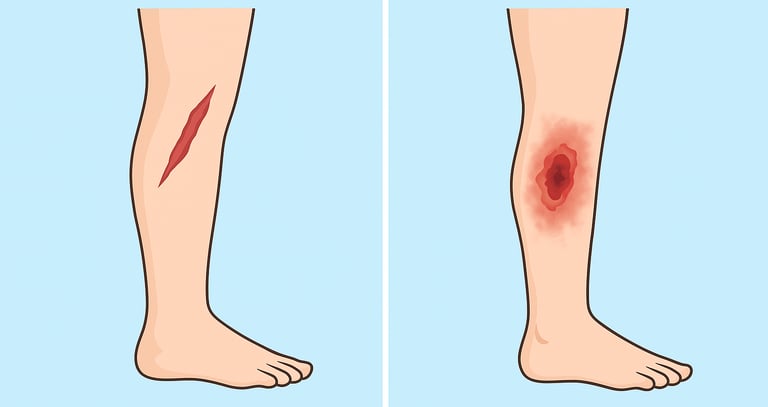

Wounds happen often, but not all wounds behave the same. Some heal quickly with basic care, while others linger, resist treatment, and require specialized care. Understanding the difference between acute wounds and chronic wounds helps clinicians, patients, and caregivers recognize when a wound needs more than just a standard dressing. Terms like delayed wound healing, chronic wound care, wound bed preparation, and advanced wound therapies are important in the wound-care industry. This article uses clear language and includes evidence-based insights and sources you can read for more depth.
What are acute wounds?
Acute wounds are injuries that disrupt the skin or underlying tissue — such as cuts, surgical incisions, burns, or abrasions — and, when managed properly, proceed through a predictable healing process. Studies describe how these wounds follow four overlapping phases: hemostasis, inflammation, proliferation (granulation and epithelialization), and then remodeling (scar formation and maturation).
Key features of acute wounds:
A known cause (trauma, surgery, thermal injury)
Rapid onset, clear timeline
In the absence of complicating factors, healing proceeds in days to weeks
Typically respond to standard first-aid and wound-care dressings
For example, a leg laceration sutured and dressed might close in two to four weeks, without significant complications. Prompt cleansing, closure, moisture balance, and protection from further trauma are usually sufficient.
What are chronic wounds?
In contrast, chronic wounds are those that fail to progress through the normal phases of healing in a timely fashion. While definitions vary, many clinical sources define a chronic wound as one that shows little improvement after 2–4 weeks of appropriate care or does not fully heal within 3 months.
Identifying features of chronic wounds:
Underlying systemic or local barrier to healing (e.g., diabetes, vascular disease, poor nutrition, repeated trauma)
Stalled healing: the wound may be stuck in inflammation, or show little contraction or epithelialization
Frequently colonised by bacterial biofilm, have excess exudate, or necrotic/poor-quality tissue bed
Higher risk of complications (infection, tissue loss, amputation) and higher resource use
A typical example: a venous leg ulcer in a person with chronic venous insufficiency, or a diabetic foot ulcer (DFU) in a patient with neuropathy and peripheral arterial disease (PAD). These wounds may persist for months without timely specialist management.
Why do acute and chronic wounds differ biologically?
Acute wounds progress through well-regulated healing phases. Chronic wounds, in contrast, get stuck in a dysfunctional microenvironment. Reviews of immunology and repair physiology highlight key differences:
In chronic wounds, the inflammatory phase fails to resolve: there is persistent inflammation with pro-inflammatory macrophages, excess matrix metalloproteinases (MMPs), high reactive oxygen species (ROS), and bacterial biofilm.
Local factors like hypoxia (low oxygen), poor perfusion, edema, and repeated trauma interfere with granulation tissue formation and remodeling.
Systemic factors — such as diabetes, vascular disease, malnutrition, immune dysfunction — can further impair cellular responses needed for healing.
Thus the wound microenvironment in chronic wounds is fundamentally different from the well-controlled repair environment of acute wounds, which explains why chronic wounds need more complex management.
Why the distinction matters in wound care
Recognizing whether a wound is acute or at risk of becoming chronic has important implications:
Assessment: chronic wounds warrant more detailed evaluation (vascular studies, neuropathy screening, nutritional assessments, infection culture) beyond simply cleaning and dressing.
Treatment planning: acute wounds generally need standard wound care (cleaning, moisture management, protection), while chronic wounds require wound-bed preparation (frequent debridement), biofilm management, advanced dressings/therapies, offloading (for DFUs), compression (for VLUs), or revascularisation (for ischemic ulcers).
Referral decisions: delayed healing (no meaningful improvement after 2–4 weeks) should prompt early referral to a specialist wound care centre rather than waiting until complications emerge.
Resource allocation: chronic wounds consume more resources (clinic time, advanced therapies, multidisciplinary input) and carry higher morbidity and cost burdens. Early intervention may reduce long-term burden.
Practical assessment checklist
When you assess any wound, ask:
Onset and timeline – When did the wound start? Has it shown measurable improvement (size reduction, less exudate) in 2–4 weeks?
Cause and risk factors – Trauma or surgery (acute) vs underlying disease (chronic risk). Are there systemic issues (diabetes, PAD, malnutrition) or local issues (high pressure, repeated trauma)?
Appearance and progress – Clean bed with granulation in acute wound; stalled bed, slough/necrosis, heavy exudate may suggest chronic.
Perfusion and innervation – Check pulses, target ABI/toe pressures for lower extremity wounds; check neuropathy for DFUs.
Infection and biofilm risk – Persistent non-healing suggests possible biofilm or infection rather than simple delay.
Nutrition and systemic status – Weight loss, low albumin, poor glycemic control, smoking, renal disease (chronic wound risk factors).
Set a timepoint for review – If no meaningful progress by 2–4 weeks of optimal local care, escalate or refer.
Summary and take-home messages
Acute wounds: timely onset, predictable progression, healing in days to weeks under appropriate care.
Chronic wounds: failing to progress through normal healing phases; associated with systemic/local barriers; require more comprehensive and advanced care.
The transition from acute to chronic is an important clinical moment. Early recognition and intervention can improve outcomes.
Treating a chronic wound means looking beyond the wound bed (debridement, dressing) to underlying causes (vascular, metabolic, nutritional, mechanical).
Use measurable milestones (e.g., 20–40 % reduction in size by 2–4 weeks) to guide decision-making.
By understanding the differences between acute and chronic wounds, clinicians and care teams can direct resources more effectively, intervene earlier, and help improve healing trajectories.
See also
What Are the Different Types of Wounds? A Practical Guide
Best Practices for Chronic Wound Care: How to Assess Foot Ulcers Effectively
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
How Often Should Wound Dressings Be Changed? Best Practices for Healing
Wound Care Guide: How to Tell Colonization from True Infection
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Krzyszczyk P, Schloss R, Palmer A and Berthiaume F (2018) The Role of Macrophages in Acute and Chronic Wound Healing and Interventions to Promote Pro-wound Healing Phenotypes. Frontiers in Physiology. 9:419. doi: 10.3389/fphys.2018.00419 https://www.frontiersin.org/articles/10.3389/fphys.2018.00419/full
Raziyeva K, Kim Y, Zharkinbekov Z, Kassymbek K, Jimi S, Saparov A. Immunology of Acute and Chronic Wound Healing. Biomolecules. 2021; 11(5):700. https://doi.org/10.3390/biom11050700 https://www.mdpi.com/2218-273X/11/5/700
Shailendra Singh, Alistair Young, Clare-Ellen McNaught, The physiology of wound healing, Surgery (Oxford),
Volume 35, Issue 9, 2017, Pages 473-477, ISSN 0263-9319, https://doi.org/10.1016/j.mpsur.2017.06.004.
https://www.sciencedirect.com/science/article/abs/pii/S0263931917301369
Frykberg RG, Banks J. Challenges in the Treatment of Chronic Wounds. Adv Wound Care (New Rochelle). 2015 Sep 1;4(9):560-582. doi: 10.1089/wound.2015.0635. PMID: 26339534; PMCID: PMC4528992. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4528992/
Sen CK. Human Wound and Its Burden: Updated 2022 Compendium of Estimates. Adv Wound Care (New Rochelle). 2023 Dec;12(12):657-670. doi: 10.1089/wound.2023.0150. PMID: 37756368; PMCID: PMC10615092. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10615092/
Han G, Ceilley R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv Ther. 2017 Mar;34(3):599-610. doi: 10.1007/s12325-017-0478-y. Epub 2017 Jan 21. PMID: 28108895; PMCID: PMC5350204. https://pmc.ncbi.nlm.nih.gov/articles/PMC5350204/
Bottaro, A. Verywell Health. “12 Reasons Your Wound Is Not Healing.” 2025. https://www.verywellhealth.com/slow-wound-healing-11683569.
Byram Healthcare. “The Difference Between Acute and Chronic Wound Care.” 2021. https://www.byramhealthcare.com/blogs/the-difference-between-acute-and-chronic-wound-care.
“Need for Improved Definition of ‘Chronic Wounds’ in Clinical Studies.” Acta Dermato-Venereologica, 2016. https://www.medicaljournals.se/acta/content/html/10.2340/00015555-2786
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
