When Is Hyperbaric Oxygen Therapy Right for Wound Care?
Learn when hyperbaric oxygen therapy is appropriate for wound care, its benefits, indications, and key clinical guidelines for optimal healing outcomes.
admin
10/20/20258 min read
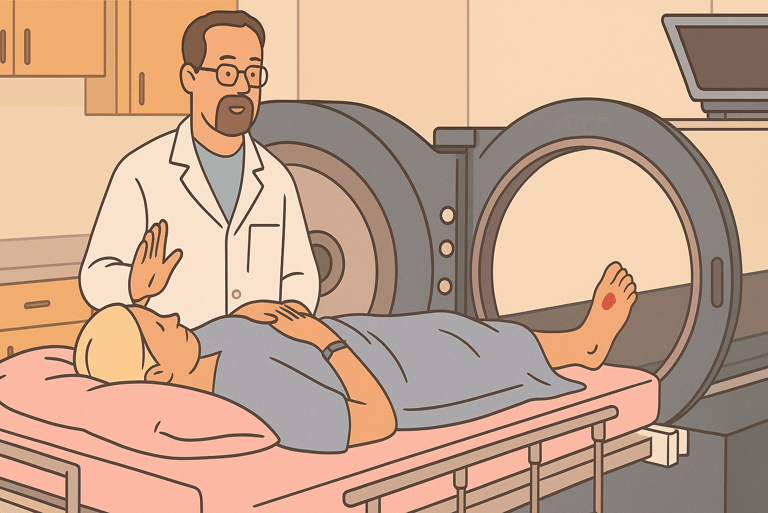
Hyperbaric oxygen therapy (HBOT), sometimes shortened to “HBO” or “HBOT”, delivers 100% oxygen to a patient inside a pressurized chamber. In wound care, HBOT is used as an adjunctive therapy to increase tissue oxygenation, reduce hypoxia, and support processes important for healing (angiogenesis, collagen formation, infection control). But HBOT is not for every wound, and the decision to refer a patient requires weighing evidence, patient factors, logistics, and risks. This guide explains when HBOT may be helpful, which wound types are most commonly considered, practical patient-selection criteria, what the evidence actually shows, and how to combine HBOT with standard wound-care practices.
When HBOT is plausible
HBOT is most often considered for chronic, non-healing foot ulcers in people with diabetes that have not responded to optimal standard care (debridement, infection control, offloading, revascularization when indicated), especially when ischemia or severe hypoxia is present and when limb salvage is an active goal. Professional societies also recognize HBOT for certain refractory soft-tissue or bone infections (e.g., refractory osteomyelitis), radiation-induced tissue injury, and other specific indications. Evidence shows short-term benefits for some diabetic foot ulcers and possible reductions in major amputation for selected patients, but the quality and consistency of studies vary and long-term outcomes are less clear.
How HBOT might help wounds
HBOT increases the amount of dissolved oxygen in plasma by combining high inspired oxygen fraction with increased atmospheric pressure inside a chamber. Higher tissue oxygen levels can:
Improve neutrophil and macrophage function and help fight infection.
Promote angiogenesis (new blood vessel growth) and collagen deposition.
Reduce tissue edema through vasoconstriction while maintaining or increasing oxygen delivery.
Enhance the effect of some antibiotics and support graft or flap survival.
These physiologic effects help explain why HBOT can be useful for hypoxic or ischemic wounds and certain infections, but clinical benefit depends on patient selection, timing, and concurrent management.
Conditions where HBOT is commonly considered
Major professional bodies and the literature list several wound-related conditions where HBOT is an option, usually as an adjunct to standard care:
Diabetic foot ulcers (DFUs) that are chronic, deep, or ischemic and that have not responded to several weeks of optimal therapy. Some trials show more rapid short-term healing and possible amputation reduction in selected patients. Guidelines recommend referral for HBOT after standard measures (including revascularization when needed) have been applied and healing is not progressing.
Refractory osteomyelitis (persistent bone infection despite surgery and antibiotics). HBOT may be used adjunctively in some centers.
Radiation-induced tissue injury (late radiation necrosis of soft tissue or bone). HBOT has a more established role for selected late radiation injuries (e.g., mandibular osteoradionecrosis).
Compromised grafts or flaps where improved oxygenation might support tissue survival.
Other complex or ischemic wounds where poor tissue oxygenation is a major barrier and other treatments have been optimized.
Note: UK NICE guidance and several guideline panels urge caution and selective use; HBOT is not a routine first-line therapy for all DFUs or chronic wounds.
What the evidence shows
Systematic reviews and Cochrane analyses find that HBOT can improve short-term healing of diabetic foot ulcers and may reduce the risk of major amputation in some trials, but many studies are small, heterogeneous, and have design limitations. Consequently, confidence in long-term benefits and broad generalization is limited.
Recent systematic reviews (2021–2025) continue to report promising signals — faster ulcer reduction and fewer amputations in selected populations — while also calling for more high-quality, adequately powered randomized trials and better reporting. Some newer analyses highlight better outcomes when HBOT is added after meticulous standard-of-care measures and when patient selection is careful.
Guidelines (e.g., IWGDF and specialty societies) generally recommend considering HBOT for diabetic foot ulcers that fail to heal despite optimal care, rather than offering it routinely; local policies and access often shape real-world use. The Undersea and Hyperbaric Medical Society (UHMS) lists diabetic wounds among accepted indications for HBOT when criteria are met.
In plain language: HBOT may help some patients with difficult-to-heal, hypoxic wounds, especially diabetic foot ulcers after other treatments have been tried, but it is not a universal cure and the strength of evidence varies.
Practical patient-selection checklist
Before referring a patient for HBOT, consider this checklist. HBOT is more likely to be appropriate when most or all of these things are true:
Diagnosis & problem: Chronic foot ulcer (often diabetic) or other wound with objective evidence of poor healing after an adequate trial (usually several weeks) of standard care (debridement, offloading, infection control, appropriate dressings).
Optimized systemic care: Glycemic control, nutrition, vascular status assessed and addressed (revascularization performed when indicated). HBOT is an adjunct; it works best when the root causes are managed.
Wound characteristics: Evidence of hypoxia/ischemia, large or deep wounds (Wagner grade 3+ in some protocols), or wounds complicated by refractory infection/osteomyelitis after surgery/antibiotics.
Feasibility and access: Patient can tolerate multiple daily treatments (often 20–40 sessions), has no absolute contraindication (untreated pneumothorax, some pulmonary barotrauma risks), and can attend chamber sessions.
Multidisciplinary agreement: Wound team, vascular surgery, infectious disease, and hyperbaric medicine specialists agree HBOT is a reasonable adjunct in this case.
If these items are not met, HBOT is less likely to be effective and other interventions should be prioritized.
Typical HBOT course and logistics
Treatment schedule: Many protocols use daily sessions (5–7 days/week) at pressures of about 2.0–2.5 ATA for ~90 minutes (with air breaks) over 20–40 sessions, although exact regimens vary. Some centers tailor course length to clinical response.
Monitoring and integration: HBOT is delivered alongside standard wound care — debridement, dressings, offloading, antibiotics, and revascularization as needed. Clinical response is monitored at regular intervals; if no improvement after an adequate course, clinicians reconsider the plan.
Access: HBOT requires a dedicated chamber (monoplace or multiplace), trained staff, and safety systems; access varies by region and health system. Cost and reimbursement policies (including Medicare/LCD decisions and UHMS indications) influence availability.
Safety and contraindications
HBOT is generally well tolerated but has potential risks:
Barotrauma to ears or sinuses (most common), and rarely middle-ear or pulmonary barotrauma.
Oxygen toxicity leading to seizures is rare at standard therapeutic settings but possible; staff monitor oxygen exposure.
Claustrophobia or discomfort during sessions can limit tolerance.
Relative contraindications include untreated pneumothorax; careful assessment is needed for those with severe pulmonary disease or uncontrolled seizure disorders.
Careful patient selection, pre-treatment evaluation, and experienced HBOT centers minimize these risks.
Cost-effectiveness and health-system considerations
HBOT can be resource-intensive. Some economic analyses suggest adjunctive HBOT may be cost-effective in preventing major amputations in selected patients (because limb salvage has major downstream savings and quality-of-life benefits), but findings depend on local costs, patient selection, and the strength of clinical benefit in specific populations. Decision-makers often require strict referral criteria and multidisciplinary approval before funding HBOT.
How to discuss HBOT with patients (suggestions)
“HBOT provides extra oxygen to the wound inside a special chamber. It may help certain hard-to-heal, low-oxygen wounds that haven’t improved with other treatments.”
“HBOT is an add-on, not a replacement. We’ll make sure blood flow, infection, and wound care are optimized before considering it.”
“If recommended, it involves daily sessions over weeks, some people feel ear pressure or mild discomfort, and we monitor closely for safety.”
Bottom line
HBOT can be useful for selected patients with diabetic foot ulcers or other ischemic/refractory wounds, particularly when wounds are hypoxic, have failed optimal standard care, and limb salvage is the goal.
HBOT should be considered after multidisciplinary review, optimization of vascular status and infection control, and when patients can tolerate the course and commute to a certified HBOT center.
The evidence shows short-term healing benefits and possible amputation reduction in selected trials, but study quality varies and long-term benefit is less certain. Further high-quality trials are still needed.
See also
When to Use Skin Substitutes or Grafts for Non-Healing Wounds
Stem Cells, Exosomes, and Biologics: Do They Work in Wound Care?
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
Why Diabetic Foot Wounds Heal Slowly: Top Factors That Delay Recovery
How Often Should Wound Dressings Be Changed? Best Practices for Healing
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Chen P, et al. Guidelines on interventions to enhance healing of foot ulcers in people with diabetes. International Working Group on the Diabetic Foot (IWGDF). https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-2023-07-Wound-Healing-Guideline.pdf
Kranke P, Bennett MH, Martyn‐St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD004123. DOI: 10.1002/14651858.CD004123.pub4. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004123.pub4/full
UHMS — Indications for Hyperbaric Oxygen Therapy. Undersea & Hyperbaric Medical Society. https://www.uhms.org/resources/featured-resources/hbo-indications.html
Hanley ME, Manna B. Hyperbaric Treatment of Diabetic Foot Ulcer. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430783/
Damineni U, Divity S, Gundapaneni S, et al. (February 06, 2025) Clinical Outcomes of Hyperbaric Oxygen Therapy for Diabetic Foot Ulcers: A Systematic Review. Cureus 17(2): e78655. doi:10.7759/cureus.78655
https://www.cureus.com/articles/336309-clinical-outcomes-of-hyperbaric-oxygen-therapy-for-diabetic-foot-ulcers-a-systematic-review#!/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11890413/Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD004123. DOI: 10.1002/14651858.CD004123.pub4. https://www.cochrane.org/evidence/CD004123_hyperbaric-oxygen-therapy-treating-chronic-wounds
Wenhui L, Changgeng F, Lei X, Baozhong Y, Guobin L, Weijing F. Hyperbaric oxygen therapy for chronic diabetic foot ulcers: An overview of systematic reviews. Diabetes Research and Clinical Practice. 2021 Jun;176:108862. doi: 10.1016/j.diabres.2021.108862. Epub 2021 May 17. PMID: 34015392.
https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(21)00221-7/abstract
https://pubmed.ncbi.nlm.nih.gov/34015392/Éric Senneville, Zaina Albalawi, Suzanne A van Asten, Zulfiqarali G Abbas, Geneve Allison, Javier Aragón-Sánchez, John M Embil, Lawrence A Lavery, Majdi Alhasan, Orhan Oz, Ilker Uçkay, Vilma Urbančič-Rovan, Zhang-Rong Xu, Edgar J G Peters, IWGDF/IDSA Guidelines on the Diagnosis and Treatment of Diabetes-related Foot Infections (IWGDF/IDSA 2023), Clinical Infectious Diseases, 2023;, ciad527, https://doi.org/10.1093/cid/ciad527
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciad527/7287196NICE evidence appendix and review references. National Institute for Health and Care Excellence. https://www.nice.org.uk/guidance/ng17/evidence/appendix-a4-summary-of-evidence-from-surveillance-ng19-pdf-6837997940
Oley MH, Oley MC, Kepel BJ, Faruk M, Wagiu AMJ, Sukarno I, Tulong MT, Sukarno V. Hyperbaric Oxygen Therapy for Diabetic Foot Ulcers Based on Wagner Grading: A Systematic Review and Meta-analysis. Plastic & Reconstroctive Surgery - Global Open. 2024 Mar 25;12(3):e5692. doi: 10.1097/GOX.0000000000005692. PMID: 38528847; PMCID: PMC10962882. https://journals.lww.com/prsgo/fulltext/2024/03000/hyperbaric_oxygen_therapy_for_diabetic_foot_ulcers.59.aspx
https://pmc.ncbi.nlm.nih.gov/articles/PMC10962882/Ortega MA, Fraile-Martinez O, García-Montero C, Callejón-Peláez E, Sáez MA, Álvarez-Mon MA, García-Honduvilla N, Monserrat J, Álvarez-Mon M, Bujan J, Canals ML. A General Overview on the Hyperbaric Oxygen Therapy: Applications, Mechanisms and Translational Opportunities. Medicina (Kaunas). 2021 Aug 24;57(9):864. doi: 10.3390/medicina57090864. PMID: 34577787; PMCID: PMC8465921. https://pmc.ncbi.nlm.nih.gov/articles/PMC8465921/
Huang E, et al. 2015. A clinical practice guideline for the use of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers. Undersea & Hyperbaric Medical Society.
https://www.uhms.org/images/CPG/UHM_42-3_CPG_for_DFU.pdf.Zhiming Zhang, Wenjing Zhang, Yuqi Xu, Dewu Liu. Efficacy of hyperbaric oxygen therapy for diabetic foot ulcers: An updated systematic review and meta-analysis, Asian Journal of Surgery, Volume 45, Issue 1, 2022, Pages 68-78, ISSN 1015-9584, https://doi.org/10.1016/j.asjsur.2021.07.047 https://www.sciencedirect.com/science/article/pii/S1015958421004644
Myrthong A L, Gurav S, Mahankudo S, et al. (December 02, 2024) Hyperbaric Oxygen Therapy Combined With Standard Wound Care Versus Standard Wound Care Alone in Patients With Diabetic Foot Ulcers: A Prospective Comparative Study. Cureus 16(12): e74964. DOI 10.7759/cureus.74964 https://www.cureus.com/articles/313684-hyperbaric-oxygen-therapy-combined-with-standard-wound-care-versus-standard-wound-care-alone-in-patients-with-diabetic-foot-ulcers-a-prospective-comparative-study.pdf.
Ken Mackay, Rhiannon Thompson, Matthew Parker, James Pedersen, Hayden Kelly, Mairi Loynd, Emily Giffen, Angus Baker. The role of hyperbaric oxygen therapy in the treatment of diabetic foot ulcers - A literature review, Journal of Diabetes and its Complications, Volume 39, Issue 3, 2025, 108973, ISSN 1056-8727, https://doi.org/10.1016/j.jdiacomp.2025.108973
https://www.sciencedirect.com/science/article/pii/S1056872725000261.
UCLA Health — HBOT indications and patient information. https://www.uclahealth.org/medical-services/hyperbaric/indications.
Huang ET. UHMS Hyperbaric Medicine Indications Manual (15th ed). 2023. Undersea & Hyperbaric Medical Society. https://www.uhms.org/images/indications/UHMS%20Indications%2015th%20Ed%20Front%20Matter%20and%20References.pdf. uhms.org
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
