What Are the Different Types of Wounds? A Practical Guide
Learn about acute vs. chronic wounds and key wound types (pressure injuries, diabetic foot ulcers, venous leg ulcers, burns, and more) to support proper wound care.
admin
10/24/20256 min read
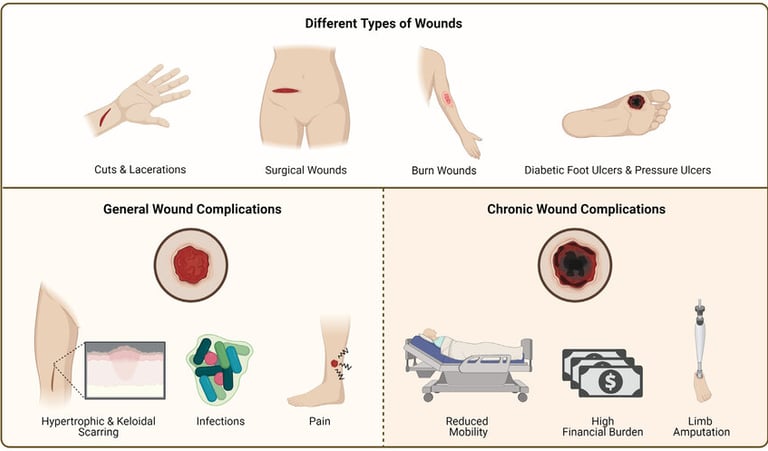
Wounds come in many shapes and sizes. Some are acute and heal quickly with simple care; others are chronic and need specialist attention. Knowing the common wound types, and the basic differences between them, helps clinicians and patients choose the right assessment, treatment, and follow-up plan.
Two big categories: acute vs chronic wounds
Wounds are often grouped first by how they behave over time.
Acute wounds result from a specific injury (cut, surgical incision, or burn) and usually heal through an orderly sequence in days to weeks if there’s no major complication. Examples: surgical incisions, traumatic lacerations, and many burns.
Chronic wounds fail to progress through normal healing in an expected timeframe (commonly defined in practice as not showing meaningful improvement after 4–12 weeks). Chronic wounds include diabetic foot ulcers (DFUs), venous leg ulcers (VLUs), and many long-standing pressure injuries. Chronic wounds often reflect underlying problems such as poor blood flow, neuropathy, infection, or nutrition deficits.
Understanding which category a wound falls into is the first step in planning care.
1. Traumatic wounds (acute)
These are wounds caused by sudden physical force: cuts, abrasions, puncture wounds, and lacerations from accidents. Key points:
Assessment looks for depth, contamination, and damage to underlying structures (tendons, nerves, vessels).
Management focuses on bleeding control, cleansing, tetanus status, and appropriate closure (sutures, adhesives, or leaving open if contaminated).
Most heal predictably, but heavily contaminated or deep wounds may become infected or require specialist repair.
2. Surgical wounds (incisions)
Surgical wounds are intentional breaks in the skin created during an operation. They are usually clean and closed at surgery, but complications can occur:
Uncomplicated surgical incisions heal by primary intention when edges are approximated.
Surgical-site infections (SSI) can develop and require antibiotics, drainage, or debridement.
Postoperative wound care includes incision checks, dressing changes, and instructions about signs of infection.
3. Pressure injuries/pressure ulcers
Pressure injuries happen where prolonged pressure (often combined with shear) damages skin and underlying tissue, typically over bony prominences (heels, sacrum). The National/International Pressure Injury panels use a staging system (stage 1–4, plus unstageable and deep tissue injury) to describe severity and depth. Early identification and offloading are central to prevention and treatment.
4. Diabetic foot ulcers (DFUs) and neuropathic wounds
People with diabetes commonly develop foot wounds because of peripheral neuropathy, foot deformities, repetitive pressure, and sometimes poor circulation. DFUs carry a higher risk of infection and limb loss than many other wounds, so early specialist involvement is often recommended. Management centers on debridement, offloading, infection control, vascular assessment, and optimizing blood glucose.
5. Venous leg ulcers (VLUs)
Venous ulcers typically appear on the lower leg between the knee and ankle in people with chronic venous insufficiency. They are often shallow but stubbornly chronic, with heavy exudate and irregular edges. Compression therapy (when not contraindicated) and treatment of venous disease are mainstays of care.
6. Arterial (ischemic) ulcers
Arterial ulcers result from poor blood flow (peripheral arterial disease) and often occur on the toes or pressure points. They tend to be painful, have a “punched-out” appearance, and may be accompanied by cool skin and diminished pulses. Vascular assessment (ABI, toe pressures, duplex) and revascularization when feasible are key to improving healing chances.
7. Burns (classified by depth and extent)
Burns are classified by depth (superficial/superficial partial-thickness, deep partial-thickness, full-thickness) and by total body surface area (TBSA) involved. Depth drives management: superficial burns often heal with conservative care, while deep partial and full-thickness burns may need grafting and specialized burn center care. Thermal, chemical, electrical, and radiation burns each have unique considerations.
8. Other specialized wound types
Fungal or atypical infectious wounds: e.g., mycobacterial or fungal infections that require targeted microbiology and antimicrobial therapy.
Malignant or neoplastic wounds: cancer-related skin breakdown requires oncology input and palliative wound strategies.
Autoimmune or vasculitic ulcers: these stem from systemic inflammatory disorders and often need systemic therapy in addition to local wound care.
Moisture-associated skin damage (MASD): caused by prolonged exposure to urine, stool, sweat, or wound exudate; management emphasizes skin protection and moisture control.
Why correct classification matters
Calling a wound by the right type matters because it directs diagnostics (e.g., vascular studies for ischemic wounds, neuropathy testing for DFUs), immediate therapies (offloading, compression, revascularization), and when to refer to specialists (vascular surgery, burn center, infectious disease, wound clinic). Misclassification can delay effective treatment and increase complication risk.
Quick practical tips for clinicians
Measure and photograph wounds at baseline and follow-up to document progress.
Screen for perfusion (pulses, ABI/toe pressures) in nonhealing lower-extremity wounds.
Consider early referral for wounds that are deep, increasingly painful, exposed bone/tendon, infected, or not improving after 2–4 weeks of appropriate care.
Address systemic contributors: glycemic control, nutrition, smoking cessation, and medications that impair healing.
See also
Best Practices for Chronic Wound Care: How to Assess Foot Ulcers Effectively
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
Why Diabetic Foot Wounds Heal Slowly: Top Factors That Delay Recovery
How Often Should Wound Dressings Be Changed? Best Practices for Healing
Wound Care Guide: How to Tell Colonization from True Infection
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Armstrong DG, Tan T, Boulton AJM, Bus SA. Diabetic Foot Ulcers: A Review. JAMA. 2023;330(1):62–75. doi:10.1001/jama.2023.10578 https://pmc.ncbi.nlm.nih.gov/articles/PMC10723802/
https://jamanetwork.com/journals/jama/article-abstract/2806655Żwierełło W, Piorun K, Skórka-Majewicz M, Maruszewska A, Antoniewski J, Gutowska I. Burns: Classification, Pathophysiology, and Treatment: A Review. Int J Mol Sci. 2023 Feb 13;24(4):3749. doi: 10.3390/ijms24043749. PMID: 36835171; PMCID: PMC9959609. https://pmc.ncbi.nlm.nih.gov/articles/PMC9959609/
Vasudevan, Biju. Venous leg ulcers: Pathophysiology and Classification. Indian Dermatology Online Journal 5(3):p 366-370, Jul–Sep 2014. | DOI: 10.4103/2229-5178.137819 https://pmc.ncbi.nlm.nih.gov/articles/PMC4144244/
https://journals.lww.com/idoj/fulltext/2014/05030/venous_leg_ulcers__pathophysiology_and.39.aspxEdsberg, Laura E.; Black, Joyce M.; Goldberg, Margaret; McNichol, Laurie; Moore, Lynn; Sieggreen, Mary. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. Journal of Wound, Ostomy and Continence Nursing 43(6):p 585-597, November/December 2016. | DOI: 10.1097/WON.0000000000000281
https://pmc.ncbi.nlm.nih.gov/articles/PMC5098472/
https://journals.lww.com/jwocnonline/fulltext/2016/11000/revised_national_pressure_ulcer_advisory_panel.3.aspxWarby R, Maani CV. Burn Classification. [Updated 2023 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539773/
Jais S. Various Types of Wounds That Diabetic Patients Can Develop: A Narrative Review. Clinical Pathology. 2023;16. doi:10.1177/2632010X231205366 https://pmc.ncbi.nlm.nih.gov/articles/PMC10566271/
https://journals.sagepub.com/doi/10.1177/2632010X231205366Kavitha KV, Tiwari S, Purandare VB, et al. Choice of wound care in diabetic foot ulcer: A practical approach. World Journal of Diabetes. 2014 Aug;5(4):546-556. DOI: 10.4239/wjd.v5.i4.546. PMID: 25126400; PMCID: PMC4127589. https://europepmc.org/article/pmc/4127589
Bernatchez SF, Eysaman-Walker J, Weir D. Venous Leg Ulcers: A Review of Published Assessment and Treatment Algorithms. Adv Wound Care (New Rochelle). 2022 Jan;11(1):28-41. doi: 10.1089/wound.2020.1381. Epub 2021 Apr 13. PMID: 33848433; PMCID: PMC8573799. https://pmc.ncbi.nlm.nih.gov/articles/PMC8573799/
https://www.liebertpub.com/doi/10.1089/wound.2020.1381NPIAP Pressure Injury Stages. National Pressure Injury Advisory Panel (NPIAP) https://cdn.ymaws.com/npiap.com/resource/resmgr/online_store/npiap_pressure_injury_stages.pdf
Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Hong JP, Katsanos K, Mills JL, Nikol S, Reekers J, Venermo M, Zierler RE, Schaper NC; International Working Group on the Diabetic Foot (IWGDF). Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3276. doi: 10.1002/dmrr.3276. Epub 2020 Jan 20. PMID: 31958217. https://pubmed.ncbi.nlm.nih.gov/31958217/
https://iwgdfguidelines.org/wp-content/uploads/2020/11/Hinchliffe_et_al-2020-IWGDF-PAD-guideline.pdfProcedure: NPUAP Staging System for Pressure Injuries (Updated 2016). South West Regional Wound Care Program. https://www.swrwoundcareprogram.ca/uploads/contentdocuments/hcpr%20-%20npuap%20pu%20staging%20procedure.pdf
Kim J. The pathophysiology of diabetic foot: a narrative review. J Yeungnam Med Sci. 2023;40(4):328-334.
https://www.e-jyms.org/journal/view.php?number=2810
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.














