The Role That Comorbidities Play in Delayed Wound Healing
Discover how diabetes, vascular disease, and malnutrition impact delayed wound healing, plus key wound care strategies to improve patient outcomes.
10/23/20259 min read


Chronic wounds are rarely just a local skin problem, they’re usually a symptom of wider health issues. Comorbidities such as diabetes, peripheral arterial disease (PAD) + other vascular problems, and malnutrition frequently interfere with the normal phases of wound healing and are common drivers of delayed wound healing. Understanding how these conditions interact with the wound bed helps clinicians prioritize diagnostics, choose effective treatments, and escalate care when necessary.
This article explains how diabetes, vascular disease, and poor nutrition slow healing, which clinical signs to watch for, how to assess risk, and key steps to reduce delay.
The big picture: how comorbidities impair healing
Wound healing is an ordered process (hemostasis → inflammation → proliferation → remodeling). Comorbid conditions commonly disrupt one or more phases:
They can reduce blood flow and oxygen delivery (vascular disease, PAD), so tissues lack the oxygen needed for cell proliferation and infection control.
They may cause abnormal cellular responses (diabetes leads to persistent inflammation, impaired macrophage/keratinocyte/fibroblast function, and reduced angiogenesis).
They often create nutrient and protein deficits needed for collagen synthesis and immune defense (malnutrition increases complication risk and delays closure).
Because most chronic wounds occur in older or multimorbid patients, more than one of these problems commonly coexists and acts together to slow or arrest healing.
Diabetes and delayed wound healing
How diabetes interferes with repair
People with diabetes are at high risk for chronic wounds, particularly diabetic foot ulcers (DFUs). Diabetes can slow healing through several mechanisms:
Hyperglycemia-related microvascular damage reduces capillary blood flow and oxygen delivery.
Peripheral neuropathy reduces protective sensation. Patients may not feel minor trauma, allowing small sores to progress before detection.
Impaired immune response and chronic inflammation. High glucose and metabolic changes alter neutrophil and macrophage function and promote a prolonged inflammatory state that prevents normal progression to the proliferative phase.
Cellular dysfunction. Fibroblasts, keratinocytes, and endothelial cells in diabetic wounds often have reduced migration, proliferation, and angiogenic responses.
Clinical consequences and clues
DFUs may be deep, recurrent, and slow to epithelialize. Loss of protective sensation (tested by monofilament), decreased pulses or cool skin, and a history of prior ulcers/amputation should raise concern for combined neuropathy and vascular disease.
What to do clinically
Optimize glycemic control as part of a comprehensive plan.
Perform regular foot inspections in at-risk patients and educate about early reporting of breaks in skin.
Refer early to multidisciplinary diabetic foot services if a DFU is deep, infected, ischemic, or not improving within a few weeks. Guidelines emphasize integrated care for best outcomes.
Peripheral arterial disease (PAD) and other vascular disorders
How vascular disease delays healing
Wounds need oxygen and nutrients; arterial disease reduces delivery:
Macrovascular obstruction (PAD) limits blood flow to distal tissues, reducing oxygen tension and nutrient supply needed for collagen formation and immune function. Without adequate perfusion, even well-managed wounds may not heal.
Microvascular dysfunction may also occur (especially with diabetes), compounding the problem.
Clinical signs of ischemia to watch for
Absent or diminished pedal pulses, delayed capillary refill, cool skin, and dependent rubor. Non-healing ulcers on the toes or forefoot, rest pain, or tissue loss are red flags. Simple bedside tests (ABI, toe pressures) help screen for PAD.
What helps
Early vascular assessment (ABI, toe pressures, duplex ultrasound) for non-healing wounds is important; timely revascularization when indicated can substantially improve healing prospects. Collaboration with vascular specialists is associated with better outcomes.
Malnutrition and specific nutrient deficits
Why nutrition matters
Wound repair is metabolically expensive. Key points:
Energy and protein needs rise in the presence of a large or infected wound; inadequate intake limits collagen synthesis and new tissue formation. Chronic wounds may increase protein requirements substantially.
Certain micronutrients (vitamin C, zinc, arginine, vitamin A, and vitamin D) play defined roles in collagen crosslinking, immune function, and cell proliferation. Deficiency or insufficiency can slow healing.
Clinical signals of malnutrition
Unintentional weight loss, low BMI, muscle wasting, poor oral intake, and laboratory indicators (low albumin or prealbumin; though these are influenced by inflammation) suggest nutritional risk. Screening tools (MUST, NRS-2002) help identify patients who need dietitian assessment.
Interventions
Nutritional assessment and support are recommended for patients with chronic or complicated wounds. Oral nutritional supplements (high-protein formulas, arginine-enriched ONS) and targeted micronutrient repletion (when deficiency is identified) can support healing as an adjunct to wound care. Guidelines such as ESPEN emphasize individualized support.
Other comorbidities that matter
While diabetes, PAD, and malnutrition are major drivers, other conditions commonly delay healing:
Chronic kidney disease (CKD) affects immune function and tissue repair and is associated with poorer wound outcomes.
Heart failure and poor cardiac output may limit peripheral perfusion.
Chronic obstructive pulmonary disease (COPD) and smoking reduce tissue oxygenation and increase complication risk.
Immunosuppression (steroids, chemotherapy, HIV) increases infection risk and slows granulation.
Recognizing these comorbidities helps clinicians predict slower trajectories and justify earlier specialist input.
How comorbidities interact
Most patients with chronic wounds have more than one risk factor. For example, a person with diabetes may have neuropathy, PAD, and malnutrition — each contributes a different barrier to healing (poor sensation, poor perfusion, and insufficient substrate for tissue synthesis). Studies of prognostic factors consistently show worse outcomes when multiple comorbidities are present. Clinical care should therefore be multidisciplinary and multimodal.
Practical clinical approach: assess, optimize, escalate
Assess thoroughly
Document wound size, depth, tissue types, exudate, odor, and pain. Take high-quality photos and serial measurements. Screen for neuropathy, pulses, ABI or toe pressures, and nutritional risk. Order basic labs (CBC, CRP/ESR, glucose/HbA1c, renal function) as indicated.
Optimize systemic factors
Improve glycemic control, stop smoking, treat anemia, and correct nutrition deficits. Initiate specialist referrals (vascular, endocrinology, dietitian, infectious disease) when indicated.
Provide wound-focused care
Debride devitalized tissue, manage exudate with appropriate dressings, control infection, and offload pressure (for DFUs) or apply compression for venous ulcers. Use NPWT, skin substitutes, or HBOT selectively based on guideline indications and after addressing comorbid contributors.
Escalate early
If there is no measurable improvement after a reasonable trial (often 2–4 weeks of optimized local care), escalate to a specialized wound clinic for multidisciplinary assessment. Early vascular evaluation is especially important for ischemic-appearing wounds.
Patient and system-level implications
Patient education and self-care (foot inspections for people with diabetes, smoking cessation, and dietary support) help prevent wounds and catch problems early.
Multidisciplinary wound services — combining vascular surgery, podiatry, infectious disease, wound nursing, and dietetics — generally provide the best pathway to address interacting comorbidities. Evidence shows earlier specialist involvement improves diagnostic accuracy and access to revascularization when needed.
Limitations
Research on comorbidities and wound outcomes is strong on associations and mechanisms but variable in quantifying exact risks for every patient. Individual responses differ. The recommendations above reflect evidence from guideline bodies, systematic reviews, and mechanistic studies, but they are not absolute rules. Clinical judgment and multidisciplinary input remain essential.
Key takeaways
Comorbidities commonly cause delayed wound healing. Diabetes (neuropathy + impaired cell function), PAD (reduced perfusion), and malnutrition (lack of protein and micronutrients) are frequent and modifiable contributors.
Screen and treat systemically, not just locally. Address glycemic control, vascular status, and nutrition as part of wound care.
Use a multidisciplinary approach and consider early specialist referral when wounds are deep, ischemic, infected, or not improving after 2–4 weeks of optimized care.
See also
The Role of Nutrition in Wound Care: Best Foods for Healing
When to Refer a Patient to a Wound Care Center: Key Guidelines
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
Why Diabetic Foot Wounds Heal Slowly: Top Factors That Delay Recovery
How Often Should Wound Dressings Be Changed? Best Practices for Healing
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Dasari N, Jiang A, Skochdopole A, Chung J, Reece EM, Vorstenbosch J, Winocour S. Updates in Diabetic Wound Healing, Inflammation, and Scarring. Seminars in Plastic Surgery. 2021 Aug;35(3):153-158. doi: 10.1055/s-0041-1731460. Epub 2021 Jul 15. PMID: 34526862; PMCID: PMC8432997. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8432997/
Bolton L. Peripheral arterial disease: Scoping review of patient-centred outcomes. International Wound Journal. 2019 Dec;16(6):1521-1532. doi: 10.1111/iwj.13232. Epub 2019 Oct 9. PMID: 31597226; PMCID: PMC7948906. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7948906/
Clark RK, Stampas A, Kerr KW, Nelson JL, Sulo S, Leon-Novelo L, Ngan E, Pandya D. Evaluating the impact of using a wound-specific oral nutritional supplement to support wound healing in a rehabilitation setting. Int Wound J. 2023 Jan;20(1):145-154. doi: 10.1111/iwj.13849. Epub 2022 Jun 9. PMID: 35684975; PMCID: PMC9797929. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9797929/
Chen P, et al. Guidelines on interventions to enhance healing of foot ulcers in people with diabetes (2023 update). International Working Group on the Diabetic Foot. https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-2023-07-Wound-Healing-Guideline.pdf
Marques R, Lopes M, Ramos P, Neves-Amado J, Alves P. Prognostic factors for delayed healing of complex wounds in adults: A scoping review. Int Wound J. 2023 Sep;20(7):2869-2886. doi: 10.1111/iwj.14128. Epub 2023 Mar 14. PMID: 36916415; PMCID: PMC10410354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10410354/
Wang R, Gu S, Kim YH, Lee A, Lin H, Jiang D. Diabetic Wound Repair: From Mechanism to Therapeutic Opportunities. MedComm (2020). 2025 Sep 29;6(10):e70406. doi: 10.1002/mco2.70406. PMID: 41030912; PMCID: PMC12477442. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12477442/
J. Nordanstig, C.A. Behrendt, A.W. Bradbury, G.J. de Borst, FGR Fowkes, J. Golledge, A. Gottsater, R.J. Hinchliffe, S. Nikol, L. Norgren, Peripheral arterial disease (PAD) – A challenging manifestation of atherosclerosis, Preventive Medicine, Volume 171, 2023, 107489, ISSN 0091-7435, https://doi.org/10.1016/j.ypmed.2023.107489. https://www.sciencedirect.com/science/article/pii/S0091743523000695
Emanuele Cereda, J.C.L. Neyens, R. Caccialanza, M. Rondanelli, J.M.G.A. Schols,
Efficacy of a disease-specific nutritional support for pressure ulcer healing: A systematic review and meta-analysis, The Journal of nutrition, health and aging, Volume 21, Issue 6, 2017, Pages 655-661, ISSN 1279-7707, https://doi.org/10.1007/s12603-016-0822-y.
https://www.sciencedirect.com/science/article/pii/S1279770723001793
Sen CK. Human Wound and Its Burden: Updated 2022 Compendium of Estimates. Advances in Wound Care (New Rochelle). 2023 Dec;12(12):657-670. doi: 10.1089/wound.2023.0150. PMID: 37756368; PMCID: PMC10615092. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10615092/
https://www.liebertpub.com/doi/10.1089/wound.2023.0150Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(S1):e3276. https://doi.org/10.1002/dmrr.3276.
https://iwgdfguidelines.org/wp-content/uploads/2020/11/Hinchliffe_et_al-2020-IWGDF-PAD-guideline.pdfMolnar JA, Underdown MJ, Clark WA. Nutrition and Chronic Wounds. Adv Wound Care (New Rochelle). 2014 Nov 1;3(11):663-681. doi: 10.1089/wound.2014.0530. PMID: 25371850; PMCID: PMC4217039. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4217039/
https://www.liebertpub.com/doi/10.1089/wound.2014.0530Katherine J. Desneves, Bree E. Todorovic, Ann Cassar, Timothy C. Crowe,
Treatment with supplementary arginine, vitamin C and zinc in patients with pressure ulcers: A randomised controlled trial, Clinical Nutrition, Volume 24, Issue 6, 2005, Pages 979-987, ISSN 0261-5614, https://doi.org/10.1016/j.clnu.2005.06.011.
https://www.sciencedirect.com/science/article/abs/pii/S0261561405001056
https://www.clinicalnutritionjournal.com/article/S0261-5614(05)00105-6/abstractSundaram, Saranya, et al. Benefits of early vascular provider involvement in wound care center management of patients with underlying arterial disease. Journal of Vascular Surgery. 2024. Volume 80, Issue 4. p1239-1250.e1. doi: 10.1016/j.jvs.2024.05.011
https://www.jvascsurg.org/article/S0741-5214(24)01188-1/fulltext.
Nidhi Yadu, Manju Singh, Deependra Singh, S. Keshavkant,
Mechanistic insights of diabetic wound: Healing process, associated pathways and microRNA-based delivery systems, International Journal of Pharmaceutics, Volume 670, 2025, 125117, ISSN 0378-5173,
https://doi.org/10.1016/j.ijpharm.2024.125117.
https://www.sciencedirect.com/science/article/abs/pii/S0378517324013516
International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International. 2022. https://woundinfection-institute.com/wp-content/uploads/IWII-CD-2022-web-1.pdf.
Gomes F, et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clinical Nutrition. 2018. doi: 10.1016/j.clnu.2017.06.025
https://www.espen.org/files/ESPEN-Guidelines/ESPEN_guidelines_on_nutritional_support_for_polymorbid_internal_medicine_patients.pdf
https://www.clinicalnutritionjournal.com/article/S0261-5614(17)30236-4/fulltextCalvo-Wright MdM, Álvaro-Afonso FJ, López-Moral M, García-Álvarez Y, García-Morales E, Lázaro-Martínez JL. Is the Combination of Plain X-ray and Probe-to-Bone Test Useful for Diagnosing Diabetic Foot Osteomyelitis? A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(16):5369. https://doi.org/10.3390/jcm12165369. https://www.mdpi.com/2077-0383/12/16/5369
Senneville É, Albalawi Z, van Asten SA, Abbas ZG, Allison G, Aragón-Sánchez J, Embil JM, Lavery LA, Alhasan M, Oz O, Uçkay I, Urbančič-Rovan V, Xu ZR, Peters EJG. IWGDF/IDSA guidelines on the diagnosis and treatment of diabetes-related foot infections (IWGDF/IDSA 2023). Diabetes Metab Res Rev. 2024 Mar;40(3):e3687. doi: 10.1002/dmrr.3687. Epub 2023 Oct 1. PMID: 37779323. https://pubmed.ncbi.nlm.nih.gov/37779323/. https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3687
Redmond MC, Gethin G, Finn DP. A Review of Chronic Wounds and Their Impact on Negative Affect, Cognition, and Quality of Life. Int Wound J. 2025 Aug;22(8):e70748. doi: 10.1111/iwj.70748. PMID: 40819659; PMCID: PMC12358188. https://pmc.ncbi.nlm.nih.gov/articles/PMC12358188/
Ju M, Kim Y, Seo KW. Role of nutrition in wound healing and nutritional recommendations for promotion of wound healing: a narrative review. Ann Clin Nutr Metab. 2023;15(3):67-71.
https://e-acnm.org/journal/view.php?doi=10.15747/ACNM.2023.15.3.67
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
vascular sonogram
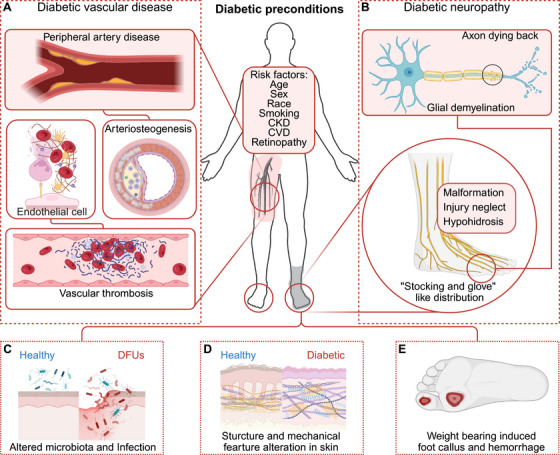
Contributing factors in diabetes leading to DFUs [MedComm]
