Protease in Wound Care: What It Is, Why It Matters, and How to Manage It
Discover how elevated protease levels impact chronic wound healing and why protease-modulating treatments are becoming essential in modern wound care.
admin
10/28/20259 min read
Proteases are enzymes that break down proteins. In wounds, proteases, produced by both human cells (host proteases) and bacteria (bacterial proteases), play a central role in tissue breakdown and repair. When protease activity is balanced, it helps remodel damaged tissue and clear debris. When protease activity is persistently elevated, especially in chronic wounds, it can degrade growth factors, extracellular matrix proteins (like collagen), and newly forming tissue; and that makes healing slower or stalled. This article explains the types of proteases important in wound care, how elevated protease activity (EPA) shows up in the clinic, why it matters for healing, and practical, evidence-based strategies clinicians can use to detect and manage protease imbalance.
Proteases 101: the enzymes behind tissue breakdown and remodeling
Proteases are a large family of enzymes that cleave peptide bonds in proteins. In wound biology the most commonly discussed proteases are:
Matrix metalloproteinases (MMPs): a family of zinc-dependent enzymes (for example MMP-2 and MMP-9) that degrade extracellular matrix (ECM) components and remodel tissue. MMPs are essential for normal wound healing but are tightly regulated by tissue inhibitors of metalloproteinases (TIMPs). Excessive MMP activity is associated with chronic wounds.
Serine proteases (including neutrophil elastase): produced by inflammatory cells (neutrophils) and can degrade ECM and antimicrobial peptides. In infected or highly inflamed wounds, neutrophil-derived proteases can be abundant.
Bacterial proteases: some wound pathogens secrete proteases that damage host tissue and can sustain a non-healing environment. Bacterial proteases also interfere with host protease regulation and immune defenses.
In acute wounds, proteases are activated transiently to clear debris and remodel tissue. In many chronic wounds, multiple protease types remain elevated, creating a biochemical environment that destroys growth factors, degrades collagen, and prevents stable granulation tissue from forming.
Why elevated protease activity (EPA) matters in wound care
Protease imbalance matters because it changes the wound microenvironment in ways that are directly relevant to healing and clinical decision-making:
Degrades growth factors and receptors. Growth factors (for example PDGF, TGF-β) are necessary for cell migration and tissue formation. Excessive proteases cleave these molecules and reduce their activity.
Breaks down new matrix. Collagen and other ECM proteins that form the scaffold for new tissue are broken down, preventing stable repair. Chronic wounds often show high collagenase activity.
Sustains inflammation. Protease activity is often linked to persistent neutrophilic inflammation — a self-reinforcing cycle that keeps the wound in the inflammatory phase.
Predicts non-healing. Multiple studies have found that high wound protease levels are associated with slower healing or failure to heal. Measuring or testing for EPA can help identify wounds that may need targeted intervention.
In short, EPA is a functional biomarker: it signals that the wound chemistry is hostile to healing and that interventions aimed only at surface coverage or simple dressings may be insufficient.
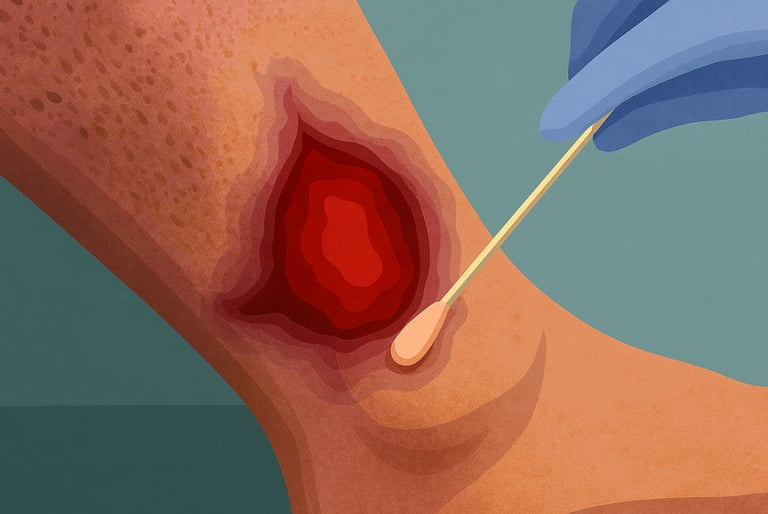
How clinicians can detect or suspect elevated protease activity
EPA is not always obvious from visual exam alone. Clinical clues include:
Poor progress despite best practice care. A wound stuck in the inflammatory phase, with little granulation tissue and persistent slough, may have EPA.
High exudate and maceration. Heavy, protease-rich fluid can macerate surrounding skin and indicate biochemical imbalance.
Failure of advanced therapies that rely on growth factors or skin substitutes. If growth-factor therapies or skin grafts fail repeatedly, protease degradation may be a cause.
Point-of-care options and lab measures:
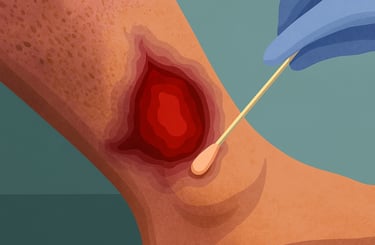
Protease activity tests (POC). Commercial lateral-flow tests (for example WOUNDCHEK™ Protease Status) are available that detect elevated inflammatory protease activity in wound fluid and can give rapid, bedside results to help guide care. NICE (UK) and some clinical groups have described the test’s intended use as a way to identify EPA. Clinical studies have used protease tests to stratify wounds and to guide protease-modulating therapy.
Laboratory analysis of wound fluid. Research labs can assay MMPs and elastase but this is not widely available in routine practice. Novel collection techniques and standardized assays have been described.
Testing can help clinicians decide whether to prioritize protease-modulating treatments over other interventions.
Evidence: protease levels and clinical outcomes
A growing body of evidence links EPA with slower healing and poorer outcomes:
Observational and cohort studies have repeatedly found higher MMP and neutrophil elastase levels in chronic wounds (venous leg ulcers, diabetic foot ulcers, pressure injuries) compared with acute wounds or healing wounds.
A multicenter randomized trial and other clinical studies have explored the use of protease activity as a biomarker to predict non-healing and to test whether protease-targeted care can improve outcomes. Results suggest that EPA identifies a subgroup of wounds at higher risk of non-healing.
Interventional trials using collagen-based dressings or collagen/oxidized regenerated cellulose (ORC) matrices (for example Promogran® and similar products) showed that these dressings can bind excessive proteases (act as sacrificial substrates) and are associated with improved healing in some trials. A landmark randomized trial of an ORC/collagen dressing reported reduced protease activity and improved healing metrics in chronic wounds. Systematic reviews of collagen dressings find signals of benefit, although heterogeneity remains.
Pharmacologic MMP inhibition is complex: broad MMP blockade can impair normal remodeling. For example, studies of broad MMP inhibition show mixed effects; MMPs are required for normal repair at some stages, so non-selective systemic MMP inhibitors have safety and efficacy limits. Low-dose doxycycline (a tetracycline antibiotic with MMP-inhibitory properties) has been studied as a modulator of MMP activity with some clinical signal in small studies, but broad adoption is not universal.
Overall, the best evidence supports local, protease-modulating dressings and targeted approaches rather than indiscriminate systemic MMP blockade.
Practical strategies to manage elevated protease activity in the clinic
When EPA is suspected or confirmed, the following evidence-informed steps are commonly recommended:
Optimize wound bed preparation first. Remove necrotic tissue (sharp or appropriate debridement), treat infection, and correct perfusion and offloading issues. Debridement reduces biofilm and removes protease-rich necrotic material.
Consider protease-modulating dressings. Collagen/ORC dressings, advanced collagen matrices, or other protease-binding dressings can act as sacrificial substrates that reduce active protease levels in wound fluid and create a more favorable biochemical environment for growth factors and cells. Clinical trials and systematic reviews support their use in selected chronic wounds.
Use topical antiseptics appropriately. Reducing bacterial burden (and bacterial proteases) when infection or biofilm is suspected can help. Dressings that also manage biofilm (for example ORC/collagen with antiseptic properties) are available. Be careful not to use cytotoxic products in a way that impairs healing.
Targeted systemic options when indicated. Low-dose doxycycline or other selective MMP modulators have been studied; these may be considered in specialist settings but require context and monitoring. Broad systemic MMP blockade is not routine because MMPs are necessary for normal repair.
Monitor response and escalate. Re-test protease status where feasible or use clinical wound-healing milestones (eg. percent reduction in area at 2–4 weeks) and escalate to reconstructive options, advanced therapies, or specialist referral when protease-modulating measures and optimization do not restore a healing trajectory.
How protease testing can change clinical decisions
Point-of-care protease testing can help by:
Identifying wounds with EPA that may benefit from collagen-based or protease-binding dressings. Studies of WOUNDCHEK™ and similar assays show that a large proportion of chronic wounds test positive for EPA, and that testing can guide therapy choices.
Avoiding premature advanced therapies such as skin grafts or bioengineered tissues in a protease-rich wound that is likely to degrade those products. Treating EPA first may improve the success of subsequent advanced interventions.
Risk stratification. EPA can be a prognostic marker for non-healing and help prioritize resource allocation and follow-up intensity.
Limitations: POC tests measure a subset of inflammatory proteases (mostly neutrophil-derived) and are one tool among many; clinical context, infection status, perfusion, and comorbidities remain essential to decision making.
Common clinical scenarios and sample care pathways
Below are two simplified scenarios that illustrate how protease thinking changes care.
Scenario A — Venous leg ulcer with EPA
Presentation: 6-month VLU with heavy exudate, maceration, minimal granulation.
Actions: perform debridement, compression therapy (if not contraindicated), test for EPA; if EPA positive, apply ORC/collagen dressing per protocol and reassess protease status or wound progress in 1–2 weeks. If inflammation and exudate fall and granulation appears, continue; if not, escalate to specialist vascular assessment.
Scenario B — Diabetic foot ulcer with failed skin substitute
Presentation: DFU treated with skin substitute that partially fails and shows breakdown.
Actions: evaluate for perfusion and infection; test for EPA (and bacterial protease activity); debride and apply protease-modulating dressing, treat infection if present, and consider repeat grafting only after EPA is controlled and wound bed is optimized.
These pathways emphasize sequencing: control proteases and infection, optimize perfusion and offloading, then attempt advanced closure strategies.
Limitations, uncertainties, and areas for future research
Which protease(s) to target? MMPs and neutrophil elastase are commonly studied, but the relative importance of different proteases can vary by wound type. More selective inhibitors or targeted approaches may be advantageous.
Optimal use of POC tests. Evidence is building but more prospective trials are needed to demonstrate that routine EPA testing leads to better long-term patient outcomes and cost-effectiveness across diverse clinical settings.
Balancing protease inhibition and normal repair. Proteases are necessary at particular healing stages; blunt suppression can be harmful. The clinical challenge is to rebalance protease activity rather than completely inhibit it.
Practical takeaways for clinicians
Suspect EPA in chronic wounds with heavy exudate, persistent slough, and stalled healing.
Debride, treat infection, and optimize perfusion/offloading first.
Consider protease-modulating dressings (collagen/ORC) when EPA is suspected or confirmed.
Use point-of-care protease tests judiciously to guide therapy and prioritize resources.
Avoid indiscriminate systemic MMP blockers; consider selective approaches and specialist input when needed.
See also
How to Tell If a Wound Is Healing: Signs of Proper Wound Care Progress
Best Practices for Chronic Wound Care: How to Assess Foot Ulcers Effectively
Why Diabetic Foot Wounds Heal Slowly: Top Factors That Delay Recovery
Wound Care Guide: How to Tell Colonization from True Infection
Best Wound Dressings for High-Exudate Wounds
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Caley MP, Martins VL, O'Toole EA. Metalloproteinases and Wound Healing. Adv Wound Care (New Rochelle). 2015 Apr 1;4(4):225-234. doi: 10.1089/wound.2014.0581. PMID: 25945285; PMCID: PMC4397992. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4397992/
https://www.liebertpub.com/doi/10.1089/wound.2014.0581McCarty SM, Percival SL. Proteases and Delayed Wound Healing. Adv Wound Care (New Rochelle). 2013 Oct;2(8):438-447. doi: 10.1089/wound.2012.0370. PMID: 24688830; PMCID: PMC3842891. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3842891/
Serena TE. Development of a Novel Technique to Collect Proteases from Chronic Wounds. Adv Wound Care (New Rochelle). 2014 Dec 1;3(12):729-732. doi: 10.1089/wound.2013.0463. PMID: 25493206; PMCID: PMC4250942. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4250942/
Veves A, et al. A Randomized, Controlled Trial of Promogran (a Collagen/Oxidized Regenerated Cellulose Dressing) vs Standard Treatment in the Management of Diabetic Foot Ulcers. JAMA Surgery. 2002. doi:10.1001/archsurg.137.7.822 https://jamanetwork.com/journals/jamasurgery/fullarticle/212677
Bohn G, Liden B, Schultz G, Yang Q, Gibson DJ. Ovine-Based Collagen Matrix Dressing: Next-Generation Collagen Dressing for Wound Care. Adv Wound Care (New Rochelle). 2016 Jan 1;5(1):1-10. doi: 10.1089/wound.2015.0660. PMID: 26858910; PMCID: PMC4717509. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4717509/
Westby MJ, Dumville JC, Stubbs N, Norman G, Wong JK, Cullum N, Riley RD. Protease activity as a prognostic factor for wound healing in venous leg ulcers. Cochrane Database Syst Rev. 2018 Sep 1;9(9):CD012841. doi: 10.1002/14651858.CD012841.pub2. PMID: 30171767; PMCID: PMC6513613.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012841.pub2/full https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6513613/Serena TE, Bayliff SW, Brosnan PJ, DiMarco DT, Doner BA, Guthrie DA, Patel KD, Sabo MJ, Samies JH, Carter MJ. Bacterial protease activity as a biomarker to assess the risk of non-healing in chronic wounds: Results from a multicentre randomised controlled clinical trial. Wound Repair Regen. 2021 Sep;29(5):752-758. doi: 10.1111/wrr.12941. Epub 2021 May 31. Erratum in: Wound Repair Regen. 2021 Nov;29(6):1080. doi: 10.1111/wrr.12980. PMID: 34057796. https://pubmed.ncbi.nlm.nih.gov/34057796/
Shu H, Xia Z, Qin X, Wang X, Lu W, Luo Q, Zhang Z, Xiong X. The clinical efficacy of collagen dressing on chronic wounds: A meta-analysis of 11 randomized controlled trials. Front Surg. 2022 Aug 31;9:978407. doi: 10.3389/fsurg.2022.978407. PMID: 36117827; PMCID: PMC9473315. https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2022.978407/full https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9473315/
Mirastschijski U, Schnabel R, Claes J, Schneider W, Agren MS, Haaksma C, Tomasek JJ. Matrix metalloproteinase inhibition delays wound healing and blocks the latent transforming growth factor-beta1-promoted myofibroblast formation and function. Wound Repair Regen. 2010 Mar-Apr;18(2):223-34. doi: 10.1111/j.1524-475X.2010.00574.x. Epub 2010 Mar 12. Erratum in: Wound Repair Regen. 2011 May-Jun;19(3):453. PMID: 20409148; PMCID: PMC2859473. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2859473/
NICE Medical Technology Guidance. WOUNDCHEK™ Protease Status for assessing elevated protease status in chronic wounds. 2016. https://www.nice.org.uk/advice/mib83/chapter/the-technology
Kandhwal M, Behl T, Singh S, Sharma N, Arora S, Bhatia S, Al-Harrasi A, Sachdeva M, Bungau S. Role of matrix metalloproteinase in wound healing. Am J Transl Res. 2022 Jul 15;14(7):4391-4405. PMID: 35958464; PMCID: PMC9360851. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9360851/
Gapski R, Barr JL, Sarment DP, Layher MG, Socransky SS, Giannobile WV. Effect of systemic matrix metalloproteinase inhibition on periodontal wound repair: a proof of concept trial. J Periodontol. 2004 Mar;75(3):441-52. doi: 10.1902/jop.2004.75.3.441. PMID: 15088883; PMCID: PMC2584373. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2584373/
Hingorani DV, Lippert CN, Crisp JL, Savariar EN, Hasselmann JPC, Kuo C, et al. (2018) Impact of MMP-2 and MMP-9 enzyme activity on wound healing, tumor growth and RACPP cleavage. PLoS ONE 13(9): e0198464. https://doi.org/10.1371/journal.pone.0198464
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0198464
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
