🚨 CMS Finalizes Historic Payment Overhaul for Skin Substitutes: What You Need to Know for 2026
CMS's CY 2026 rule changes skin substitute payment to an "incident-to" supply, ending "buy and bill." Prepare for a lower, flat rate and new FDA-based categories.
admin
11/8/20254 min read


The Centers for Medicare & Medicaid Services (CMS) has finalized one of the most significant changes to advanced wound care reimbursement in years. Contained within the vast CY 2026 Physician Fee Schedule (PFS) Final Rule, these new policies fundamentally change how skin substitutes (also known as Cellular and Tissue-Based Products, or CTPs) are paid for in physician offices and certain other outpatient settings.
If you work with these products—whether you're a clinician, practice manager, or administrator—understanding these changes, effective January 1, 2026, is crucial for financial and clinical operations.
Here is a clear, simple breakdown of everything the final rule dictates for skin substitute payment.
1. The Core Policy Change:
From Biological to "Incident-To" Supply
The single most impactful change is how CMS classifies and pays for the product itself:
The Shift:
OLD WAY: Skin substitutes were generally paid for as a separately payable biological product. This meant the product was reimbursed separately from the application procedure, often at a high average sales price (ASP), which led to the "buy and bill" model and was identified by CMS as a driver of excessive spending.
NEW WAY (Effective Jan. 1, 2026): CMS will now pay for skin substitutes as an "incident-to" supply. This means the cost of the product is now bundled into the payment for the application procedure itself. It is treated like other supplies (such as sterile gauze or sutures) necessary to perform the service.
This change aims to reduce Medicare expenditures dramatically by eliminating the financial incentive tied to the price of the product.
Key Implication:
The product itself will no longer be separately billable and reimbursed at a high rate in the physician office setting (non-facility setting). The reimbursement for the entire service is determined by a newly established rate for the application procedure.
2. The New Payment Rate: A National, Flat Fee
CMS has established a new methodology for determining the payment amount for skin substitutes.
The New Rate Structure:
CMS is creating different payment categories for skin substitutes and establishing Relative Value Units (RVUs) for the new application codes.
For the initial period (starting in 2026), many products will be placed into a single category paid at a national, flat rate ($127.28) per square centimeter.
This rate is significantly lower than the historical ASP-based rates. The goal of this new, lower payment rate is to ensure that reimbursement aligns better with the actual resource costs of the product and procedure.
Impact on Provider Revenue:
The flat rate means that the price a provider pays for a skin substitute product will directly determine its profitability, or lack thereof. Practices must now carefully evaluate the purchase price of all products against the new standardized reimbursement rate.
3. Future Differentiation:
Payment Based on FDA Status
While the initial approach involves a standardized payment for many products, CMS has acknowledged that not all skin substitutes are the same. In future rulemaking, CMS intends to establish differentiated payment categories based on the product's regulatory pathway with the U.S. Food and Drug Administration (FDA).
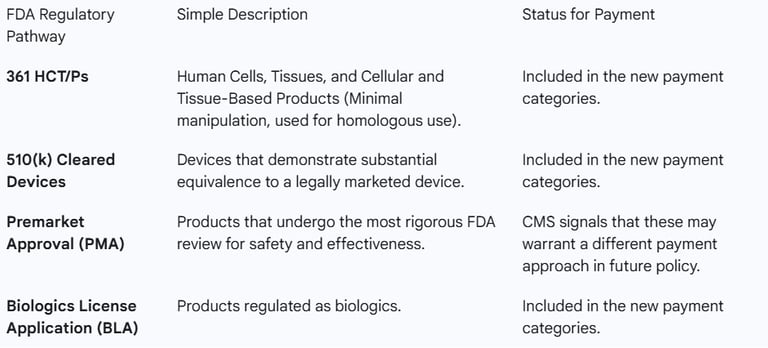
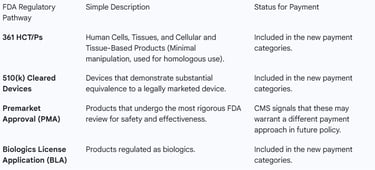
CMS categorized skin substitutes based on their regulatory pathway, which often corresponds to the level of evidence required for market entry:
Why This Matters:
By linking payment to regulatory status (especially the rigorous PMA pathway), CMS is incentivizing manufacturers to pursue the highest levels of clinical evidence to potentially qualify for a higher value payment category down the road. The new policy is designed to align payment with evidence of clinical effectiveness.
4. Setting-Specific Policies: PFS vs. OPPS
The final rule addresses payment in both the non-facility setting (physician offices) under the PFS and the hospital Outpatient Prospective Payment System (OPPS).
A. Physician Fee Schedule (PFS) – Non-Facility Setting
The Change: This is where the incident-to classification is most felt. The new payment model directly replaces the historical ASP-based payment.
Focus: The payment will be structured around new and revised procedure codes that account for the clinical labor and practice expense resources used to apply the product, with the product itself now being the "supply."
B. Outpatient Prospective Payment System (OPPS) – Hospital Setting
The Change: For products used in the hospital outpatient setting, CMS is aligning the payment methodology. Products will continue to be packaged (bundled) into the OPPS payment for the associated procedure, but the overall payment system structure aims for greater consistency across care settings.
Focus: The final rule emphasizes the need for consistency, potentially leading to a more uniform approach to how different categories of products are packaged or separately paid across both the PFS and OPPS.
5. What You Must Do Now: Actionable Steps
The CY 2026 final rule necessitates immediate changes for anyone involved in skin substitute use or billing:
Review Your Inventory and Pricing: Practices must reassess their entire skin substitute formulary. Products with a high wholesale cost that now fall into the low, national flat-rate payment category will no longer be financially viable. You must focus on cost-effective purchasing.
Focus on Utilization Efficiency: Since revenue will be driven by the procedure, not the product, successful practices will need to prioritize first-time healing success and efficient utilization. This means adhering strictly to best practices for wound bed preparation and appropriate patient selection.
Enhance Documentation: Robust documentation of medical necessity and adherence to Local Coverage Determinations (LCDs) will become even more critical to ensure all claims are paid, especially as CMS tightens the reins on utilization.
Stay Informed on Categorization: Keep a close watch for future CMS guidance on which products are assigned to which payment categories, particularly as the agency moves toward differentiating payment based on FDA evidence (PMA status).
More Information
For more information on the latest effective wound care, contact us to set up a time for a call.
Sources
Medicare and Medicaid Programs; CY 2026 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; and Medicare Prescription Drug Inflation Rebate Program
https://www.federalregister.gov/documents/2025/11/05/2025-19787/medicare-and-medicaid-programs-cy-2026-payment-policies-under-the-physician-fee-schedule-and-otherCalendar Year (CY) 2026 Medicare Physician Fee Schedule Final Rule (CMS-1832-F)
https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2026-medicare-physician-fee-schedule-final-rule-cms-1832-f
* This blog is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.